Healthcare IT Crisis Management: Preventing Equipment Failure During Patient Care
Equipment failures during patient care are a critical safety risk that 61% of healthcare organizations face regularly. From EHR crashes to printer malfunctions, these disruptions delay treatments and frustrate staff. The solution isn't reactive fixes—it's proactive IT management through standardization, real-time monitoring, clear escalation protocols, downtime testing, and preventative maintenance. Growing healthcare practices need IT systems that support care delivery, not interrupt it.

Introduction
Healthcare practices rely on technology to keep patient care moving, until that technology fails.
A printer goes offline during a lab draw.
A provider loses access to the EHR while charting.
Vital signs monitors stop syncing mid-visit.
And staff are left scrambling to troubleshoot problems they were never trained to handle.
Equipment failure during care delivery isn’t just inconvenient; it’s a patient safety risk. Yet it’s also one of the most common blind spots in small to mid-sized healthcare organizations, especially those with limited internal IT resources.
A 2023 report by the Ponemon Institute found that 61% of healthcare organizations experienced equipment or system failures that delayed care. For organizations in growth mode, adding providers, locations, or services. The risk increases as systems become more complex and harder to manage.
At Notics, we approach IT crisis management differently. While many MSPs focus on after-the-fact support, we focus on building healthcare environments that minimize the chance of failure during care. That means proactive monitoring, standardization, and real-time support built into the clinical workflow, not bolted on after something breaks.
In this article, we’ll examine the impact of equipment failure in clinical settings, outline common causes, and walk through practical steps your practice can take to prevent issues that interrupt care. Whether you're scaling from one clinic to three, or simply trying to stabilize day-to-day operations, this is where healthcare IT strategy needs to start.
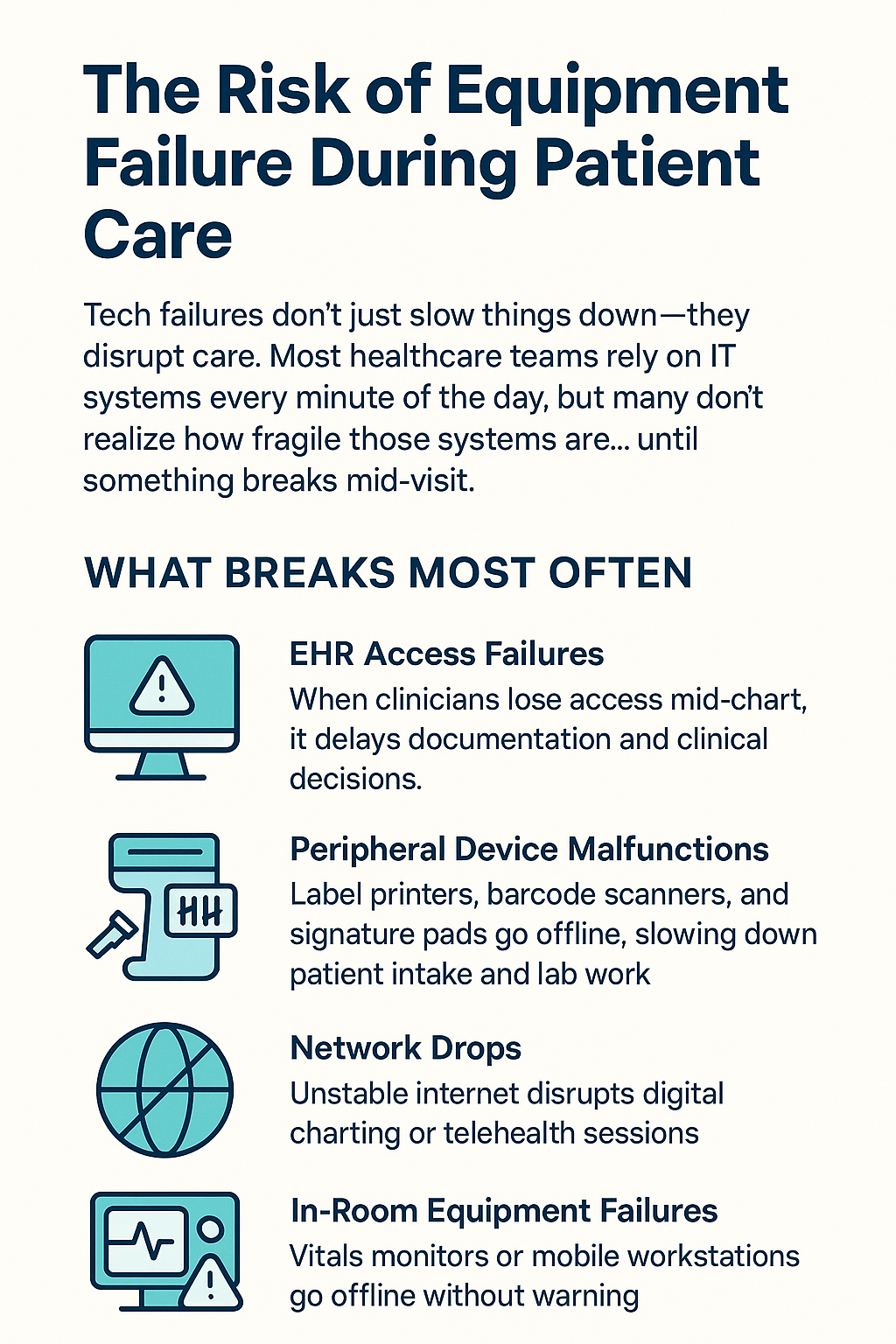
The Risk of Equipment Failure During Patient Care
Technology is deeply embedded in how healthcare gets delivered. But many organizations treat IT as a background function, until a device or system fails in the middle of care.
The most common issues include:
- EHR access failures that delay documentation or disrupt clinical decision-making
- Peripheral device malfunctions (e.g., label printers, barcode scanners, signature pads) that slow down patient intake and lab work
- Network drops that disrupt digital charting or telehealth sessions
- In-room equipment failures like vitals monitors or mobile workstations going offline without warning
These failures are often brushed off as “minor” or “temporary,” but they add up quickly.
Each disruption leads to delayed care, longer visits, frustrated staff, and. in some cases, data entry errors that affect outcomes and compliance.
For growing practices, these incidents tend to increase in frequency. More locations, more staff, and more devices mean more opportunities for breakdowns. Without proper monitoring or local support, small issues can go unresolved until they impact patient care directly.
In environments where clinicians are expected to deliver care efficiently, any tech-related slowdown becomes a risk to patient experience, regulatory compliance, and overall workflow.
Preventing Equipment Failures: 5 Steps That Make a Measurable Difference
1. Standardize and Centralize Device Management
What it is:
Using the same make and model of workstations, printers, and peripherals across all clinical areas.
Why it matters:
When equipment varies from room to room or site to site, it's harder to support, diagnose, and maintain. Standardized hardware allows IT teams to respond quickly and apply the same fixes across the board.
How to implement:
Develop a list of approved devices, and phase out unsupported or legacy models. Tie new purchases to a hardware lifecycle plan. Ensure devices are enrolled in endpoint management platforms for tracking and updates.
Business impact:
Reduces troubleshooting time, avoids inconsistent behavior, and improves support response across all clinical areas.
2. Implement Real-Time Monitoring for Critical Equipment
What it is:
Proactive monitoring tools that track the health and availability of printers, workstations, vitals machines, and networked devices.
Why it matters:
Most practices don’t discover a problem until a staff member reports it. Real-time monitoring enables IT to catch issues before they affect care.
How to implement:
Work with an MSP or internal IT partner to configure lightweight monitoring for essential clinical devices and connectivity. Prioritize uptime visibility over advanced analytics.
Business impact:
Decreases downtime, increases trust in equipment, and reduces reliance on staff to report problems after the fact.
3. Assign Local Ownership and Escalation Paths
What it is:
Clear processes for staff to report issues, and clear responsibilities for who responds.
Why it matters:
In many practices, when something breaks, no one knows who to call, or they default to overloading clinical staff with workarounds.
How to implement:
Document and communicate a tiered support plan:
- First line: who to call on-site
- Second line: when and how to contact remote support
- Emergency protocols: what to do when downtime affects care
Train staff on when to escalate and when to step away from a tech issue entirely.
Business impact:
Restores focus on care delivery and improves support response times without creating confusion.
4. Conduct Downtime Simulations and Recovery Testing
What it is:
Testing how your team handles specific device or system outages during normal operations.
Why it matters:
Most downtime protocols look good on paper but fail under pressure. Live testing ensures your practice is actually prepared.
How to implement:
Schedule quarterly or semi-annual drills that simulate printer failures, EHR lockouts, or network drops. Debrief immediately after to improve the response plan.
Business impact:
Reduces uncertainty during real failures and builds confidence across your clinical and admin teams.
5. Build Preventative Maintenance Into Daily IT Operations
What it is:
Regular updates, firmware checks, and hardware audits scheduled into your IT support cadence.
Why it matters:
Most devices don’t fail out of nowhere—they show signs first. Preventative maintenance catches them.
How to implement:
Create recurring schedules for equipment review and updates. Include critical software patches and end-of-life planning for older hardware.
Business impact:
Extends equipment lifespan, reduces emergency fixes, and ensures staff aren’t disrupted by last-minute failures.
Conclusion
IT-related equipment failure during patient care is avoidable, but only if your systems are designed to handle it.
For growing healthcare practices, where every minute of staff time counts, downtime doesn’t just slow things down. It weakens your ability to deliver consistent care.
Proactive strategies like standardization, monitoring, structured escalation, and routine maintenance aren’t optional anymore. They’re essential. Not because technology is fragile—but because your operations can’t afford to depend on luck.
At Notics, we help healthcare organizations move from reactive fixes to stable, scalable IT operations. We build systems that support care delivery, not interrupt it.
If your team is constantly working around tech issues, now’s the time to rethink how your systems are supported. The right foundation today prevents a crisis tomorrow.
🔍 Ready to assess your clinical IT risk?
Reach out for a continuity audit or to learn how on-site and remote IT support can be built into your growth plan: https://www.notics.io/solutions/healthcare
we can help
Did you enjoy this content?
Subscribe to our newsletter and get weekly tips on leveraging technology to supercharge your business operations. Don't miss out on the strategies that could transform your company!
